🔥 NIH’s $1 Trillion Failure
The Trillion Dollar Participation Trophy
With an annual budget of approximately $51 billion, the National Institutes of Health has spent over $1.1 trillion since 1970 (inflation-adjusted) (source).
Number of diseases the NIH has eradicated: Zero.
Success rate: 0.00% for complete disease elimination.
A medical politburo in Maryland deciding which of 10,000 diseases matter. Yours doesn’t.
They fund what gets published, not what saves lives.
Result: 55 million die annually while papers get published.
To be fair, eradicating disease is hard. Just ask the WHO, who eradicated smallpox for $300 million (smallpox was WHO, not NIH). Or ask Jonas Salk, who developed the polio vaccine in a university lab. Or ask the veterinarians, who’ve eradicated multiple animal diseases while the NIH was forming subcommittees.
The Translation Crisis: 166 Billion Untested Treatments
Here’s what the NIH won’t tell you:
Your grandma has Alzheimer’s in St. Louis.
- Trial-ready treatments for Alzheimer’s: Hundreds sitting on shelves
- Clinical trials available in St. Louis: Zero (for years)
- Trials on clinicaltrials.gov for your grandma: Finally, one appeared!
That one trial: - Cost: $600,000 - Purpose: A Google form survey asking if people would be interested in participating in dementia trials - Number of patients treated: Zero - Number of treatments tested: Zero
The NIH spent $600,000 researching whether people want their loved ones to get treatment.
Here’s what $600,000 could have actually funded: - 1,200 Alzheimer’s patients in pragmatic trials (at $500/patient, UK RECOVERY model) - Testing 5-10 repurposed drugs we already know are safe - Actual data on whether treatments work - Maybe saving your grandma
Instead: Meta-research. Studying whether we should do studies.
The Real Bottleneck: Geographic Gatekeeping
This isn’t a story about lack of treatments. It’s about deliberate choices not to test them:
- Potential drug combinations: 166 billion (source)
- Trial-ready Alzheimer’s treatments: Hundreds waiting
- Combinations tested annually: ~5,000
- Years to test all at current rate: 33 million
- Your disease gets tested: When the sun burns out
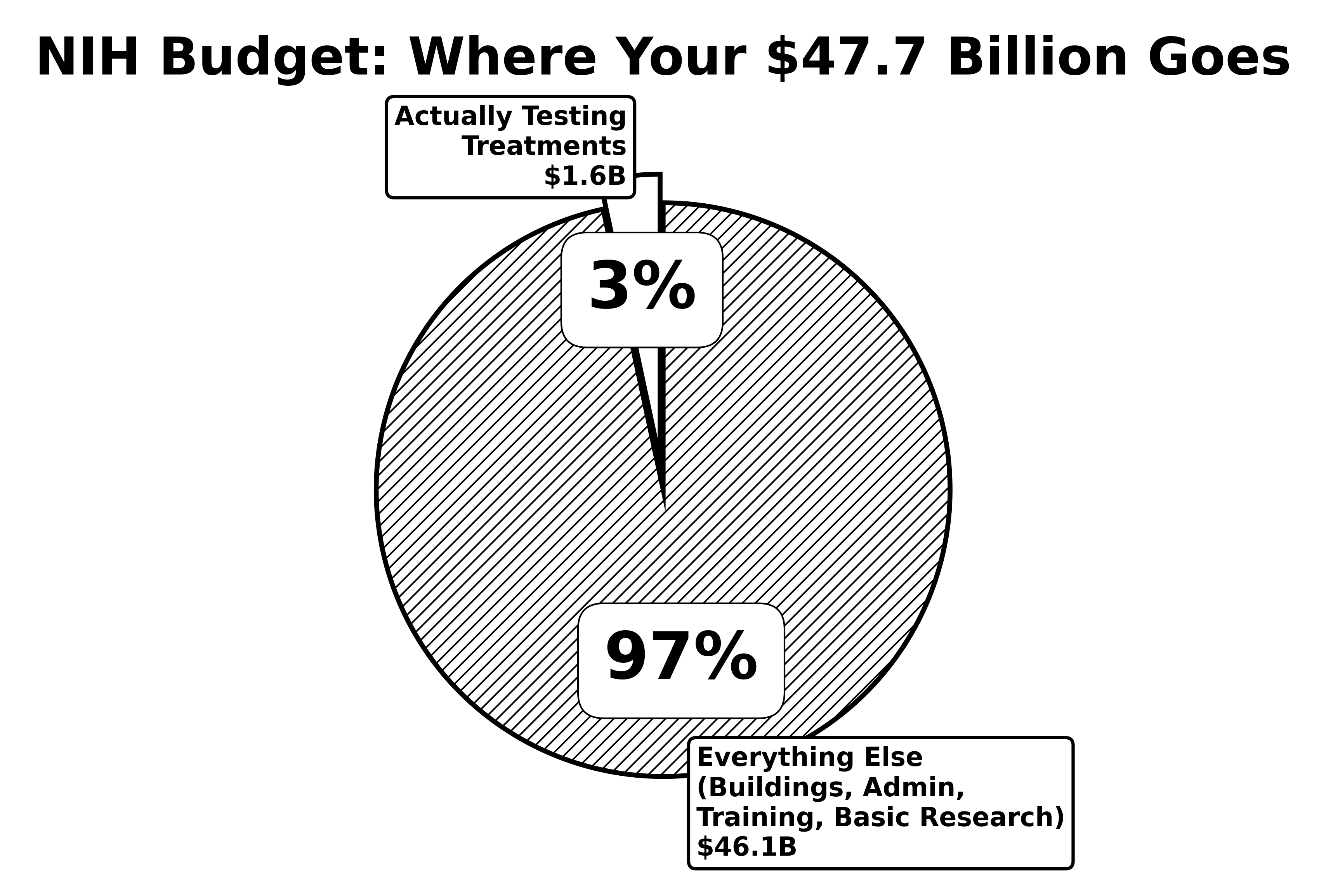
The NIH spends 55% of its budget on basic research - understanding disease mechanisms in mice.
They spend 22% on clinical trials (all types), which sounds impressive until you ask: Can your grandma in St. Louis join one?
Here’s where that 22% actually goes: - Phase 1 safety trials: Testing if drugs are safe (your grandma can’t join - wrong city, wrong age, wrong everything) - Observational studies: Watching disease progress without treatment (helpful for papers, not grandmas) - Phase 2/3 efficacy trials: Testing if treatments work (~5% of total budget) - But only in elite coastal research hospitals - Only for patients who meet 47 exclusion criteria - Never in St. Louis
The trials your grandma could actually join that might help her: ~3.3% of the NIH budget
The meta-research surveys about those trials: Apparently $600k each
Let that sink in: 55% on mice, 3.3% on trials your grandma could join.
It’s like spending your whole life studying recipes but never actually cooking anything. Then wondering why everyone’s starving.
The 85% Exclusion Zone
Even when the NIH funds trials, they systematically exclude 85% of patients (source).
Who typically can’t participate:
- Too old (most people who need medicine)
- Too sick (people who really need medicine)
- Wrong zip code (rural people)
- Taking other meds (everyone over 50)
- Not white enough (historically)
- Your rare disease child has better odds with lottery tickets
It’s like testing umbrellas only on sunny days, then wondering why they don’t work in the rain.
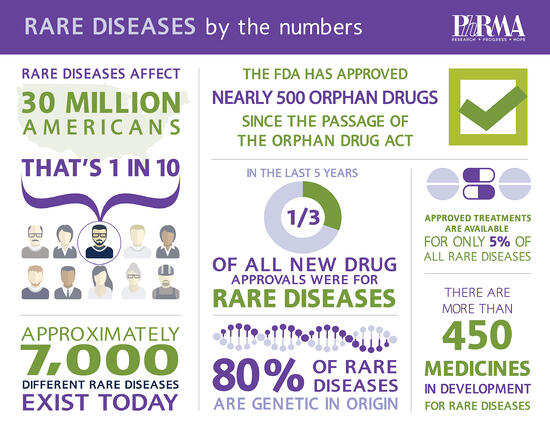
95% of diseases have ZERO approved treatments. The NIH’s official position: “Have you tried not having that disease?”
The Committee Industrial Complex
The NIH organizational chart looks like someone tried to draw the internet:
- 27 institutes and centers
- 220+ study sections (review committees)
- 6,000+ employees
- 80,000+ grant reviewers
Each institute has divisions. Each division has branches. Each branch has sections. Each section has units. It’s bureaucratic nesting dolls all the way down.
Fun fact: There are more NIH administrators than there are researchers working on some rare diseases.
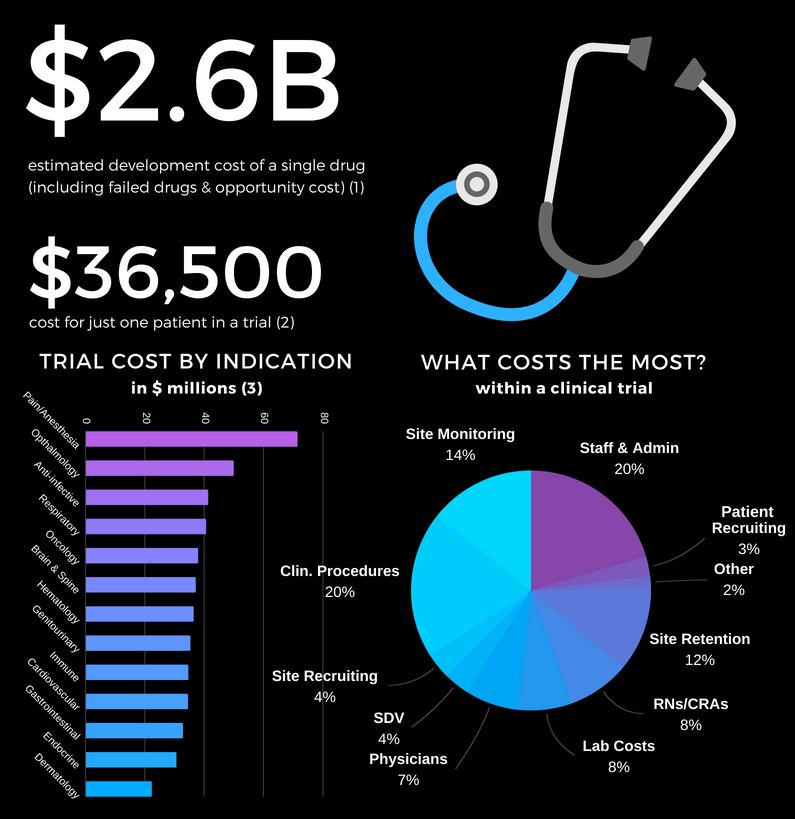
Case Study: The $1.6 Billion Long COVID Masterclass
The RECOVER Initiative - a masterpiece of inefficiency:
Budget: $1.665 billion ($1.15B + $515M in 2024) (source) Timeline: 4 years and counting Patients enrolled: ~30,000 Trials completed: Zero Cost per patient: $55,500
Meanwhile, the UK RECOVERY trial:
Budget: $20 million Timeline: 6 months Patients enrolled: 48,000 Treatments found: Multiple, including dexamethasone Cost per patient: $417
The NIH RECOVER Initiative spent 133X more per patient to achieve infinitely less (dividing by zero trials completed).
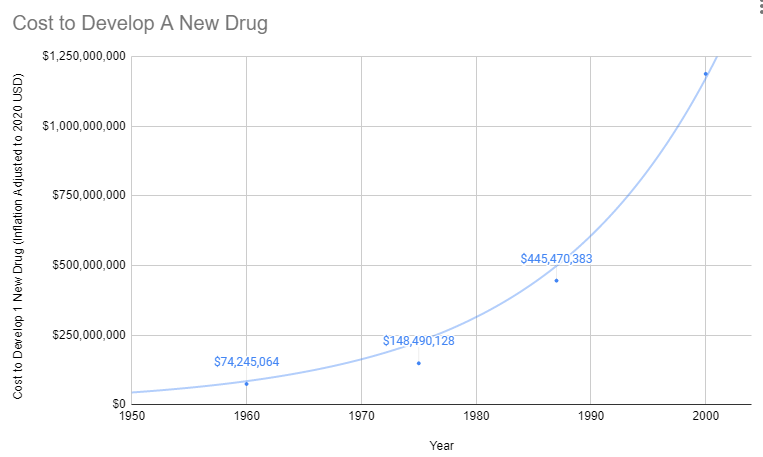
Americans Got Sicker While NIH Got Richer
“But maybe the NIH improved health in other ways!” you might say, hope flickering in your eyes.
Let’s check the scoreboard since NIH’s founding in 1887 (and massive expansion post-1970):
1970:
- Obesity rate: 13%
- Diabetes rate: 3.4%
- Life expectancy: 70.8 years
2024:
- Obesity rate: 42% (3X worse)
- Diabetes rate: 11.6% (3.4X worse)
- Life expectancy: 76.4 years (only +5.6 years, mostly from fewer people smoking)
During the NIH’s trillion-dollar spending spree, Americans got:
- Fatter
- Sicker
- More diabetic
- More depressed
- More medicated
It’s like hiring a personal trainer and gaining 100 pounds. At some point you have to wonder if they’re working for McDonald’s.
The 95% Failure Rate Nobody Talks About
Here’s a fun fact the NIH doesn’t advertise:
95% of diseases have ZERO FDA-approved treatments (source).
That’s 9,500 out of 10,000 known diseases where your treatment options are:
- Suffer
- Die
- Both
But don’t worry - the NIH formed a committee to study why their committees aren’t working.
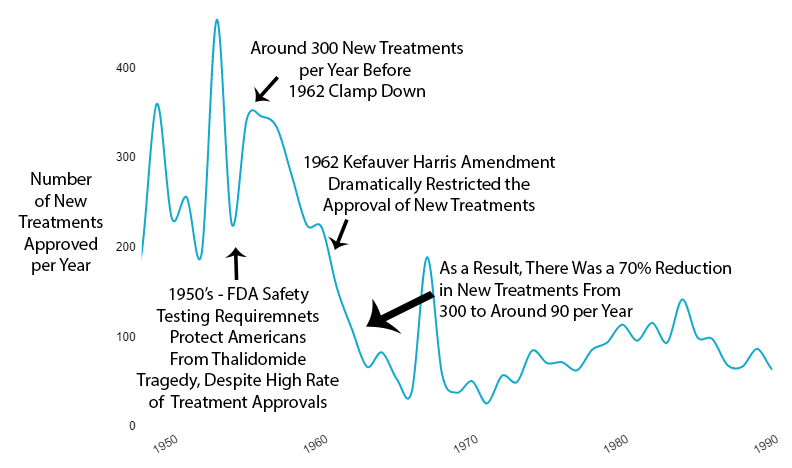
The Death Toll: 120,000 Per Decade From Delays
While the NIH debates, people die:
Deaths from regulatory delays: 120,000 per decade (source)
That’s 12,000 preventable deaths every year just from treatments stuck in bureaucracy. For context, that’s four 9/11s worth of deaths annually from paperwork.
The NIH response? Form a subcommittee to investigate whether they need a task force to study the problem.
The Basic Research Black Hole
The NIH has a dirty secret about where your money actually goes:
The Allocation Disaster:
- Basic research (mice and molecules): 55% of budget
- Clinical trials (all types): 22% of budget
- Drug development clinical trials: Only 3.3% of budget
- Phase 3 trials (the expensive ones): Only 4% of industry costs
- Papers published: 2.5 million annually
- New treatments approved: ~50 annually
- Conversion rate: 0.002%
We know everything about how cancer works in mice. We’ve mapped every pathway, gene, and protein. We have Nobel Prizes for understanding mechanisms.
What we don’t have: Cures.
Because understanding disease and curing disease are completely different things. The NIH chose understanding. Patients needed cures.
Political Funding: The Disease Popularity Contest
Which diseases get funded? Not the deadliest ones:
- Breast cancer funding: $700M/year
- Breast cancer deaths: 42,000/year
- Heart disease funding: $500M/year
- Heart disease deaths: 700,000/year
Heart disease kills 16X more people but gets less funding. Why? Pink ribbons are better at lobbying than clogged arteries.
The NIH budget is set by Congress, which means diseases compete in a popularity contest judged by people who think the immune system is a band.
Innovation Despite the NIH, Not Because of It
Major breakthroughs while NIH was busy:
- mRNA vaccines: Developed by companies, not NIH
- CRISPR: Discovered in yogurt bacteria research
- Immunotherapy: Pioneered despite medical establishment opposition
- COVID vaccines: Industry sprint while NIH planned meetings
The NIH is like that group member who shows up after the project is done to add their name.
The Efficiency Rating: An 82X Opportunity Cost
Let’s do the real math on what we could have done with that money:
Current NIH System:
- Annual budget: $51 billion
- Cost per trial participant: $41,000
- Annual participants: ~1.2 million
- Diseases cured: Zero
What $51 billion could buy using UK RECOVERY methods:
- Cost per trial participant: $500
- Annual participants: 102 million (82X more)
- Potential treatments found: Hundreds
We’re literally choosing to help 1 person badly instead of helping 82 people well.
This 82X cost disparity is the core inefficiency we can solve. (See The 82X Solution for how.)
The $2 Trillion Healthcare Burden:
Not only are we inefficient, we’re drowning:
- US-only healthcare costs: $2+ trillion annually
- Potential savings with efficient trials: $2 trillion
- Net economic swing: $4 trillion
- Untested treatments sitting on shelf: 166 billion (source)
We have more untested treatments than stars in our galaxy, but we’re too busy writing grants to test them.
The overall efficiency score:
- Input: $1.1 trillion over 50 years
- Output: Zero diseases eradicated
This results in a cost per disease cured of: \[ \text{Cost per cure} = \frac{\text{\$1.1 trillion}}{0} = \infty \]
Or, to put it another way: \[ \text{Efficiency} = \frac{\text{Diseases cured}}{\text{\$1.1 trillion}} = \frac{0}{\text{\$1.1 trillion}} = 0 \]
The NIH has achieved zero efficiency at infinite cost. That’s actually mathematically impressive.
The Patient Disconnect: Zero Correlation with Health Outcomes
Here’s the most damning statistic of all:
Correlation between NIH funding priorities and actual disease burden: 0.07
That’s essentially random. You’d get better allocation by throwing darts at a list of diseases.
What patients want:
- Treatments that work
- Access to experimental therapies
- Trials they can actually join
- Cures for their specific disease
What NIH funds:
- Understanding molecular mechanisms
- Publishing papers in prestigious journals
- Building research empires
- Protecting institutional overhead
The system optimizes for everything except patient outcomes. Because patients don’t control the money. Committees do.
What Would Actually Work
Imagine if we:
- Paid for results: Cure = payment, no cure = no payment
- Funded young scientists: When their brains still work
- Published everything: Including failures (especially failures)
- Eliminated gatekeepers: Let patients vote with participation
- Automated administration: Smart contracts > committees
But that would require admitting the current system doesn’t work. And after $1.1 trillion, that’s an expensive admission.
Fun fact: The legal framework already exists for cost recovery in trials (21 CFR 312.8). We could implement efficient trials tomorrow. But that would upset the grant-writing industrial complex.
The Bottom Line
The NIH has built the world’s most expensive grant-writing academy. They’ve turned medical research into a creative writing competition where the prize is permission to do your actual job.
For $1.1 trillion, we got:
- Millions of papers nobody reads
- Thousands of career administrators
- Hundreds of committees
- Zero eradicated diseases
But hey, at least the committees have subcommittees. And those subcommittees have working groups. And those working groups have task forces.
It’s turtles all the way down, and none of them cure cancer.
P.S. - The NIH will likely form a committee to respond to this chapter. Estimated timeline: 2-3 years for the preliminary assessment of whether a response is needed.